The Journal of Neurology & Neuropsychiatry is a leading scientific publication dedicated to advancing the understanding and treatment of neurological and neuropsychiatric disorders. As a peer-reviewed journal, it serves as a platform for researchers, clinicians, and experts to share their latest findings, innovative methodologies, and clinical experiences in the field.
This journal encompasses a broad spectrum of topics, including but not limited to neurodegenerative diseases, movement disorders, epilepsy, neuropsychiatric conditions, and neuroimaging techniques. Its interdisciplinary approach fosters collaboration between neurologists, psychiatrists, neuroscientists, and other healthcare professionals, contributing to a holistic understanding of the complexities of the brain and mind.
The Journal of Neurology & Neuropsychiatry prioritizes high-quality research that enhances diagnostic accuracy, treatment efficacy, and patient outcomes. Through the publication of original research articles, review papers, and case studies, the journal provides a comprehensive overview of the latest developments in neurology and neuropsychiatry.
Researchers and practitioners alike rely on the journal to stay informed about emerging trends, novel therapeutic interventions, and breakthroughs in neuroscientific research. The Journal of Neurology and Neuropsychiatry plays a crucial role in advancing the field, shaping clinical practices, and ultimately improving the lives of individuals affected by neurological and neuropsychiatric conditions.
| Field | Details |
|---|---|
| Title | Journal of Neurology & Neuropsychiatry |
| ISSN | Applied |
| Established (ESTD) | 2024 |
| Subject Category | Neurology, Neuropsychiatry, Brain Disorders |
| Issue Frequency | Quarterly |
| Publication Format | Fully Open Access |
| Language | English |
| Publisher Details | CLS Event & Publication |
Giuseppe Bonavina1*, Monika Zackova1, Erik Del Mestro2, Alice R. Portillo3

Juliana Bezerra Lima-Verde1, Annamaria Gomes Pereira1 and Jair Soares dos Santos1*

Levin Ace Danganan1*, Elizer Montemayor1, Renato Dejan Jr.1
Ulziizaya Sodov1*, Tovuudorj Avirmed1, Khishigsuren Zuunnast1
Valentina Colombo1*, Pamela Salucci1, Francesca Cesira Cava1, Giuseppe Bonavina1, Alice Rita Portillo1, Elisa Maietti2, Roberto Piperno3

Safaa K. H. Khalil1, W. El hotaby1, Gehan. A-R Ahmed1*, Gihan Kamel2,3 , Hadeer H.A. Sherif1, Lamyaa Abbas1
Sabina Nayab1*, Qasim Bashir2, Adnan Aslam3, Amina Saeed khan4
Paula Abola 1,*, Benjamin Wolden 1 and Mitchell Wolden1
Garrett Harris1, Chimaobi Ochulo2, and Arjun Athreya1
Keir Philip Lagrana Lope
Keren Keziah Vanguardia
Dulce Corpuz Gregorio-Talavera
Paula Abola 1* , Dita Cerina 2

Journal of Neurology & Neuropsychiatry, an open-access, peer-reviewed publication, welcomes submissions covering the entire spectrum of neurological disorder prevention, diagnosis, and treatment. Additionally, it explores topics related to molecular genetics, pathophysiology, and epidemiology in this field.

The preoperative evaluation of the function of vital organs including heart, lungs, liver and kidney is established practice across all surgical specialities. Effective perioperative evaluation and optimization has been shown to reduce postoperative medical complications, but nowadays there is a gap in the perioperative evaluation of neurological status [1]. Brain health is largerly overlooked by current modalities of perioperative assessment. On the other hand, existing protocols and guidelines focusing on modifiable risk factors for cardiac, pulmonary, renal, and metabolic-related complications have clearly demonstrated that prehabilitation strategies can decrease not only complication rates, but also 30-day mortality and length of hospital stay [2]. Frailty in the elderly population is strongly associated with the risk of postoperative complications, delirium, institutionalization, and mortality. Delirium remains the most common postoperative adverse event, with a pooled risk ratio of 2.13 (95% CI 1.23-3.67), but it can also be a marker of preclinical dementia and may contribute to delayed neurocognitive recovery [3]. It is indeed time to appreciate that surgical stress and systemic inflammation may lead to neuroinflammation, worsen preoperative neurologic status, and increase neurological complication rates in vulnerable individuals who lack physiological reserve and present with multisystemic functional deterioration. Use of Electroencephalography (EEG) monitoring as a guide to anesthetic titration to reduce the rate of perioperative cognitive disorders may prove a useful adjunct in this category of patients, but it is currently under investigation [4]. EEG is essential for differentiating delirium (a state of usually reversible global brain disfunction) and seizure disorders (a condition of spontaneous, recurrent paroxysmal electrical dysfunction), enabling the distinctly different treatment: Antiepileptic Drugs (AEDs) are a class of medications that have indeed received considerable attention as possible treatments for agitation and aggression, despite a lack of high-quality data and despite neurologist and psychiatrist often disagree on terminology.We believe that preoperative assessment of elderly and frail patients is often neglected in everyday practice but remains the foundation for a safe surgical practice. In United Kingdom, the proactive care of older patients undergoing surgery (POPS) model has integrated the Comprehensive Geriatric Assessment (CGA) in the elective and emergency surgical setting, and has provided a robust evidence based methodology to identify the elderly population at risk and to optimize the surgical pathway and the follow-up after hospital discharge [5]. A randomized clinical trial showed that preoperative CGA and optimization according to the POPS model result in fewer non-surgical complications and reduce the length of hospital stay by 40% compared to standard care [6].Normal Pressure Hydrocephalus (NPH), a condition most commonly seen in older adults is often misdiagnosed (less than 20% of patients in a Neurological unit receive an appropriate diagnosis) but has emerged as a “treatable movement disorder”, and represents a cause of delirium or cognitive decline in elderly adults who undergo cardiac surgery [7].An important aspect of perioperative care is that several drugs may have a significant impact on neurological perioperative outcomes, especially in elderly patients in whom polypharmacy is common practice. Multiple prescriptions and non-prescription medications have the potential for drug-to-drug interaction and perioperative adverse events. Although electronic health records have the potential to detect errors and interactions, having the patient bringing in all medications they use at home is a critical step at the time of office visit to prevent adverse outcomes due to drug abuse, withdrawal or interactions. Many group of drugs can cause delirium and this includes many prescriptions over the counter, complementary (“natural”) and alternative products (some examples of herbal products that have cholinergic effects are henbane, jimson weed and mandrake and some teas). The mechanism of drug induced delirium are not well defined, but evidence support a major role for cholinergic failure. Anticholinergic intoxication causes a classical delirium syndrome that may be reversible with cholinesterase inhibitors; drugs which can cause a muscarinic blockade can leads to delirium and drugs such as digoxine, lithium and histamine (H2) antagonists shoes measurable cholinergic receptor binding. The most common drugs associated with delirium are sedative hypnotics (benzodiazepines), analgesic, and medications with an anticholinergic effect. Serotoninergic drugs may also indirectly contribute to delirium by causing serotonin syndrome (in particular paroxetine due to greatest affinity for muscarinic receptors), and neuroleptic malignant syndrome [8]. This reciprocal relationship between cholinergic and dopaminergic brain effects indicate a role for dopaminergic excess in delirium and explain why dopaminergic medications such as levodopa or dopamine agonist can contribute to delirium in a dose related manner. Dopamine dysregulation syndrome and punding are encountered with levodopa therapy particularly if delivered in an intermittent fashion, with slow-release formulations and it it’s crush a slow release formulation in a nasogastric tube, as levodopa competes with amino acids for uptake in proximal small intestine. Even gastric emptying can result in erratic absorption and bioavailability. For these necessary medications, a dosage reduction or adjusting the dosage schedule may be helpful; for example, if antiparkinsonism medications are suspected of causing confusion, anticholinergic medications should be the first to be discontinued, followed by selegiline, dopamine agonist and finally and most important, by tapering levodopa, as many patients can develop an acute “akinetic attack” with hyperpyrexia and diaphoresis resembling the clinical picture of neuroleptic malignant syndrome that it may follow an abrupt change in dopaminergic medication [9-13]. Also, use of herb medications should be carefully reviewed. Patients should be counselled and monitored regarding pharmacological therapy in preparation for the surgical procedure. Deprescribing may be necessary, and alternative routes for neurotropic drug administration should be considered in the immediate postoperative period, especially after foregut procedures that may transiently impair the ability to swallow or bowel absorption.Concurrent medical problems may also contribute to “drug induced delirium”, for example in heart failure, hepatic insufficiency and renal failure; antibiotics mainly cephalosporins and macrolids may induced delirium; the mechanism behind this phenomenon is still not fully understood but has been hypothesized that may lower the seizure threshold by binding competitively to the GABA-A receptor inducing a Non-Convulsive Status Epilepticus (NCSE) manifested by an altered mental state. Frailty, rather than chronological age, is increasingly recognized as a predictor of adverse postoperative events. Interestingly, a large cohort study conducted across 9 noncardiac specialties showed that there was a greater than 10% 180-day mortality for frail patients following even low- stress procedures in low-intensity specialties [6]. This confirms that triage and optimization of preoperative assessment should be mandatory for all surgical specialties regardless of the planned procedure. Furthermore, it is time to expand the concept of pre-habilitation to include optimization of neurological functional status among the therapeutic targets. It is possible that screening for depression, anxiety, movement disorders and stroke, and a period of structured cognitive exercise along with pharmacological modulation, if necessary, can help to identify reversible deficits and strengthen the capacity of the patient to withstand surgical stress. In stroke and many neurological disorders there is impaired integrity of blood-brain barrier function, which allows more of a potentially toxic drug to reach the brain and reduced integrity of blood-brain barrier function is strongly associated with susceptibility to delirium. A comprehensive evaluation of the neurological status in elderly patients who are surgical candidates and the adoption of a collaborative neuro- geriatric perioperative care pathway could fill an existing gap, and successful treatment of delirium depend on identifying the reversible contributing factors, as drugs are the most common reversible cause of delirium. Some recent studies suggest that dexmedetomidine , a sympatholytic drug that acts as agonist to alpha-2-receptor, use for sedation in mechanically ventilated adults may reduce time to extubation in neurological disorders, may be associated with less delirium and appears to be associated with less neurocognitive dysfunction compared to other sedatives, but these findings were inconclusive because of publication bias, heterogeneity and limited sample size. These factors can improve current modalities of anesthesiological and surgical risk stratification, and reduce the risk of postoperative cognitive disorders and functional decline [11]. Finally, discharged patients form intensive care to general ward have a better neurological outcome and less subclinical delirium using the “ABCDE bundle” (Awakening and breathing coordination, delirium monitoring and exercise/early mobility”): we should investigate better if ward-transfers, arriving in the Emergency Department (ED) at nighttime, time spent in ED and visits from other specialists at nighttime could be possibly associated with development of “incident delirium” and delirium motor subtypes; the transfer of patients from the Intensive Care Unit (ICU) to a general ward can present several challenges, ensuring optimal care and reducing delirium; let us change our attitude as neurologists and clinicians, “from bed to wheelchair” [12].

This is a letter to the editor of the journal aimed at highlighting the importance that Generative Reprocessing Therapy (TRG) has gained in the last two years through the resolution of clinical cases of individuals with depression, anxiety, suicidal ideation, or fibromyalgia that have been published and report situations resolved by TRG. The reports demonstrate the effectiveness that TRG has had in improving the quality of life of these patients, where many have undergone medication tapering for these purposes. TRG has been shown to be an alternative for those cases of individuals with depression, anxiety, suicidal ideation, or fibromyalgia that cannot be resolved through conventional therapies. Further research is being conducted to better understand how this therapy works in restoring mental health.
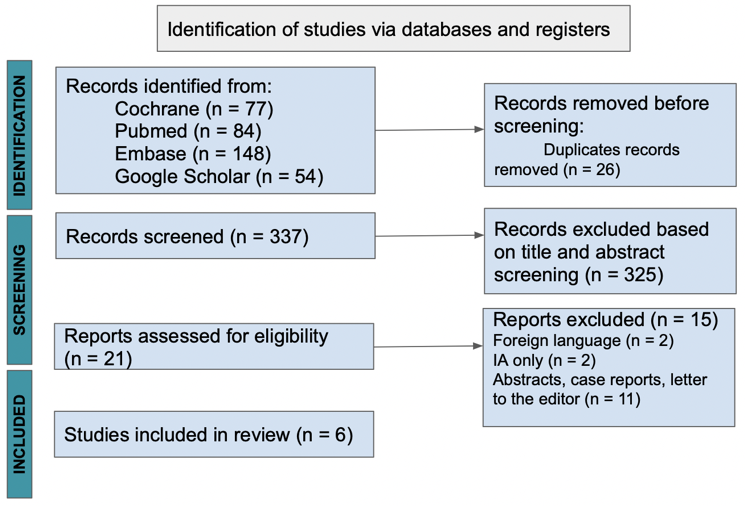
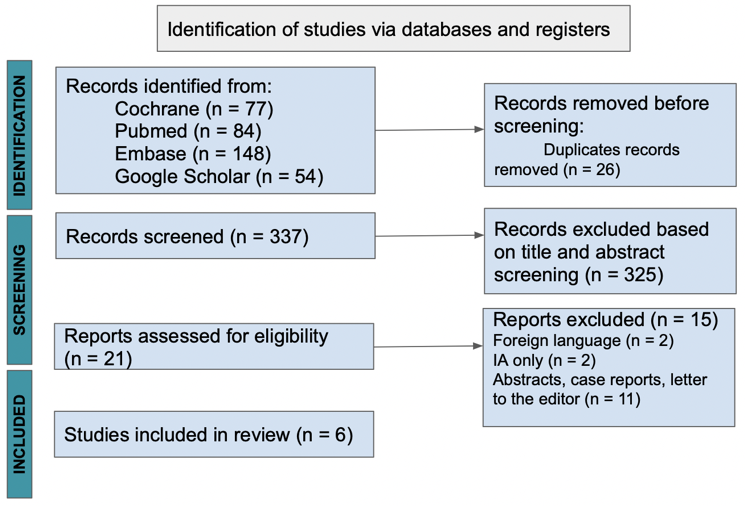
Background: Guillain-Barre Syndrome is a debilitating neurological disease with an incidence of 1.1 - 1.8 per 100,000. Autoantibodies affecting peripheral nerve membranes play an important role in understanding the pathophysiology and treatment of it. Treatment options for its cure continue to unfold and evolve. Different clinical trials resulted in increased interest in therapeutic apheresis for treatment of severe and refractory disease.Objectives: Conflicting results of immunoadsorption compared to plasma exchange in the management of Guillain-Barre Syndrome led us to synthesize available evidence from published studies. METHODS: Review Manager software was used for this review and classified the outcomes into primary (curative effect) and secondary (safety profile and relapse rate). Quality assessment and statistical data analysis were conducted using the said software.Result: The odds of achieving at least one grade disability and functional improvement was similar for patients treated with immunoadsorption and plasma exchange (OR: 0.77; 95% CI: 0.34 - 1.74; p = 0.53). Reduced risk of complications for patients treated with immunoadsorption group as compared to plasma exchange group (RR: 0.69; 95% CI: 0.43 - 1.11; p = 0.13) was noted. Increased risk of relapse for patients who underwent immunoadsorption (RR: 1.70; 95% CI: 0.96 - 3.00; p = 0.07).Conclusion: Immunoadsorption is at least as effective as plasma exchange in the treatment of Guillain-Barre Syndrome based on its curative effect by lowering its disability and improving functional score. Immunoadsorption showed reduced complications but relapse rates were higher compared to plasma exchange.
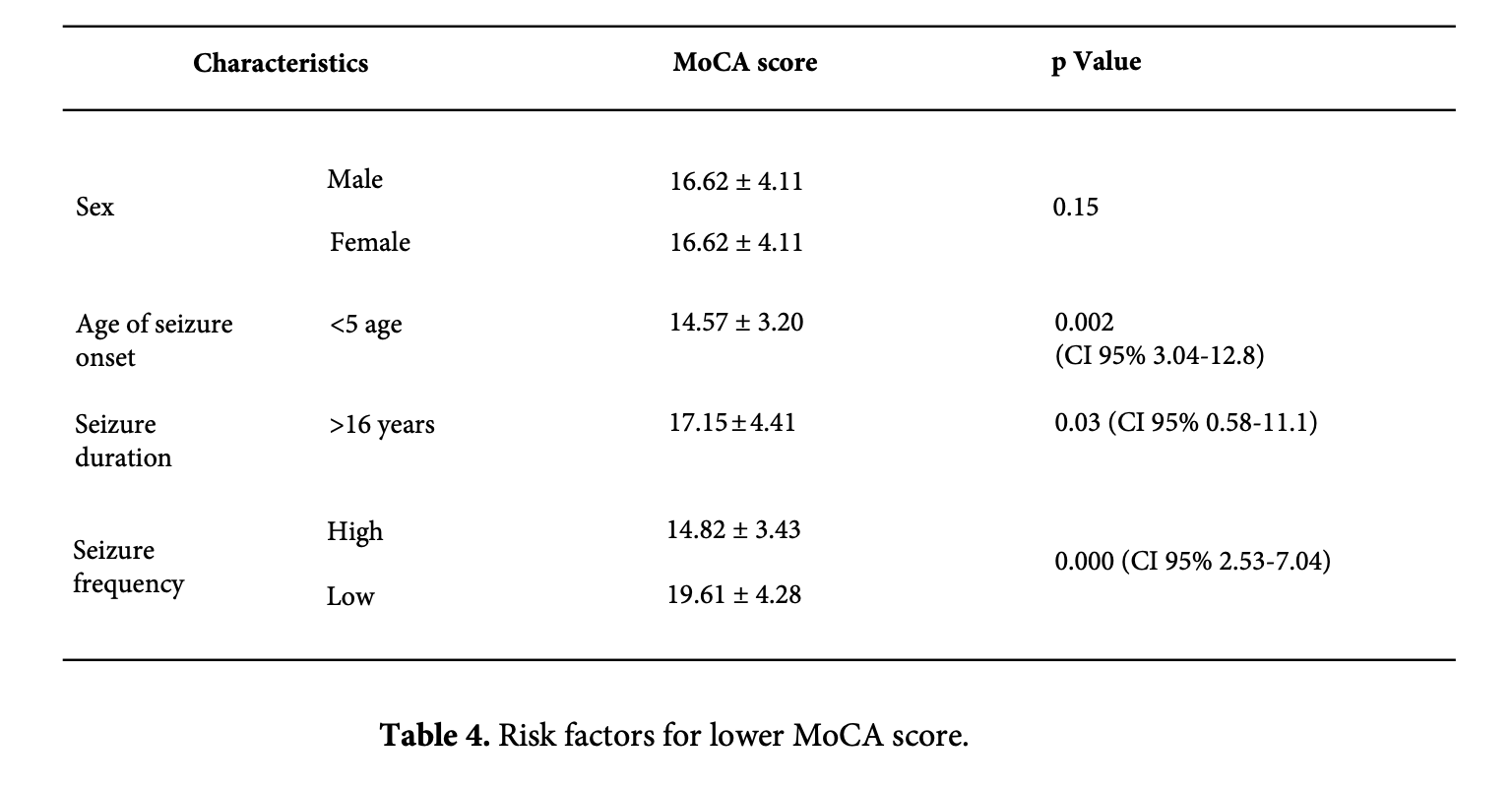
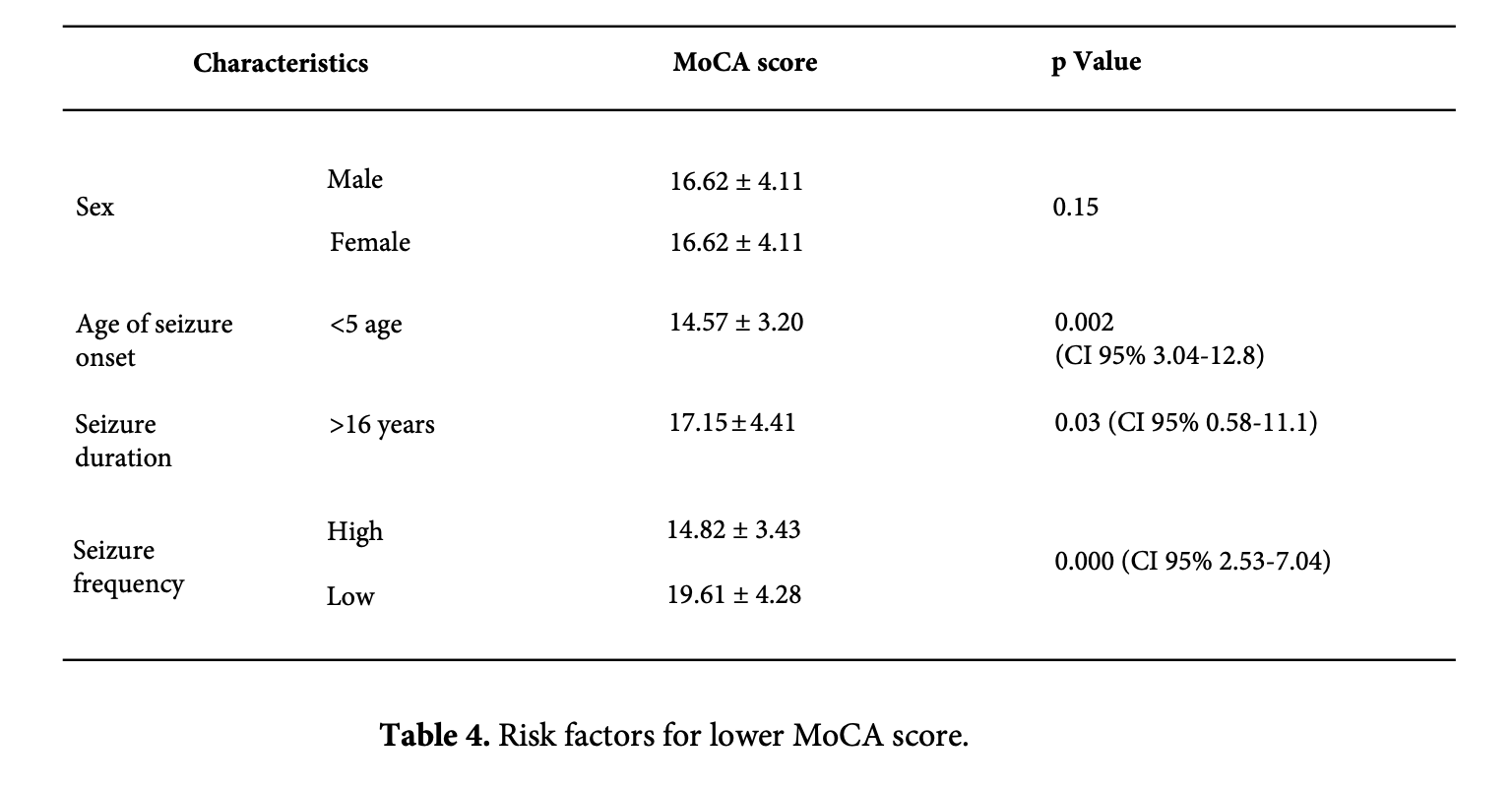
Introduction: Focal epilepsy accounts for 60% of all clinical epilepsy cases, while temporal lobe epilepsy (TLE) accounts for 40%. Cognitive impairment such as language, attention, executive function, and memory impairment are common in temporal lobe epilepsy, and researchers believe that seizure frequency and duration can cause severe hippocampal sclerosis, as well as a secondary impact on neuronal metabolism and structure, which leads to cognitive impairment. Aim: The goal is to determine the cognitive impairment of temporal lobe epilepsy, the clinical characteristics and risk factors. Materials and Methods: A cross-sectional study of 50 adults with temporal lobe epilepsy from the National Center for Mental Health used a questionnaire and Montreal Cognitive Assessment (MoCA). Results: We included 50 adults aged 26 to 61 with temporal lobe epilepsy, 52% of respondents were male, 48% were female, with an average age of 43.78±8.20 years. The study found that 92% of individuals showed cognitive impairment, with mean MoCA scores of 17.50±4.57. Long lasting seizure is a high-risk factor for cognitive function, with statistical significance (p=0.03). Seizure onset age was linked with increased attention impairments and poor visuospatial function (p=0.005), while higher seizure frequency was associated with decreased calculation (p=0.04), language (p=0.009), and drawing skills (p=0.013). Conclusion: Our study found that 58% of respondents showed moderate cognitive impairment. Low education level, earlier age of seizure onset, high seizure frequency, extended seizure duration, presence of aura, and refractory temporal lobe epilepsy all have a statistically significant effect on cognitive impairment.

AimOur study investigates the link between neuroinflammation in the olfactory bulb (OB) and Parkinson’s Disease (PD). We aim to understand how environmental factors, such as viruses and particles, trigger a cascade of events leading to ?-synuclein aggregation and the development of PD.MethodsWe conducted histological studies of PD brains, pinpointing ?-synuclein abnormalities in the anterior olfactory structures at Braak's stage 1. Our study expanded post-mortem examinations to include the OB. We assessed:The vulnerability of the olfactory epithelium and OB to inflammation, considering age-related epithelial changes.The role of microglia in the OB and their potential as a barrier against exogenous pathogens.The entry of toxins, viruses, and nanoparticles into the OB, using animal models.ResultsOur research highlights the association between viral infections and PD, including the 1918 influenza pandemic and childhood infections. Chronic rhinitis and the presence of influenza A virus in PD brains further support this link.Animal studies reveal the impact of neurotropic viruses entering via the olfactory route, leading to ?-synuclein aggregation and widespread inflammation.Activated microglia play a pivotal role in pathogen clearance but also disrupt the blood-brain barrier (BBB), particularly in the OB.Metal particles such as aluminum and iron were identified as potential contributors to PD through chronic inflammation.ConclusionThis study unveils the critical role of OB neuroinflammation as a trigger for PD. Environmental factors significantly influence PD pathogenesis, offering potential avenues for intervention and prevention. Our findings enhance the understanding of this neurodegenerative disease and open new prospects for future PD research and treatments.

SMART-ID is a widely used digital authentication application in Latvia, enabling secure access to online banking, government portals, and healthcare services [1]. While its speed and convenience have benefited the general population, its current design may unintentionally exclude a vulnerable user group: individuals living with Parkinson’s Disease (PD).In informal discussions with several people diagnosed with PD, a recurring issue was raised concerning the difficulty of entering the required PIN code in the SMART-ID app. Parkinson’s-related hand tremors, a common motor symptom, often lead to accidental mistypes during PIN entry [2]. Since the app automatically processes the code as soon as it is entered, users are not given the opportunity to review or confirm the code before it is validated. After a few incorrect attempts, the app is locked, resulting in loss of access and the need for time-consuming reactivation steps, often with assistance from others.Although the SMART-ID app complies with high security standards, current accessibility practices suggest that authentication systems should offer alternative input options or confirmatory steps to accommodate users with motor impairments [3,4]. I have contacted the SMART-ID development team and suggested a small but potentially impactful modification: introducing a manual confirmation step (e.g., an “OK” button) after PIN entry. This would allow users with motor difficulties to verify or correct their input before the system registers a failed attempt. For individuals with PD, such a design improvement could significantly reduce frustration, prevent lockouts, and promote digital independence. As healthcare systems become increasingly digitized, we must ensure that authentication tools are inclusive of those with physical or neurological disabilities [5]. While this issue may seem minor from a system perspective, it has meaningful implications for quality of life, autonomy, and equitable access to essential services.I hope this suggestion will encourage developers and digital health policymakers to consider accessibility-enhancing features in authentication apps, not only in Latvia but globally.
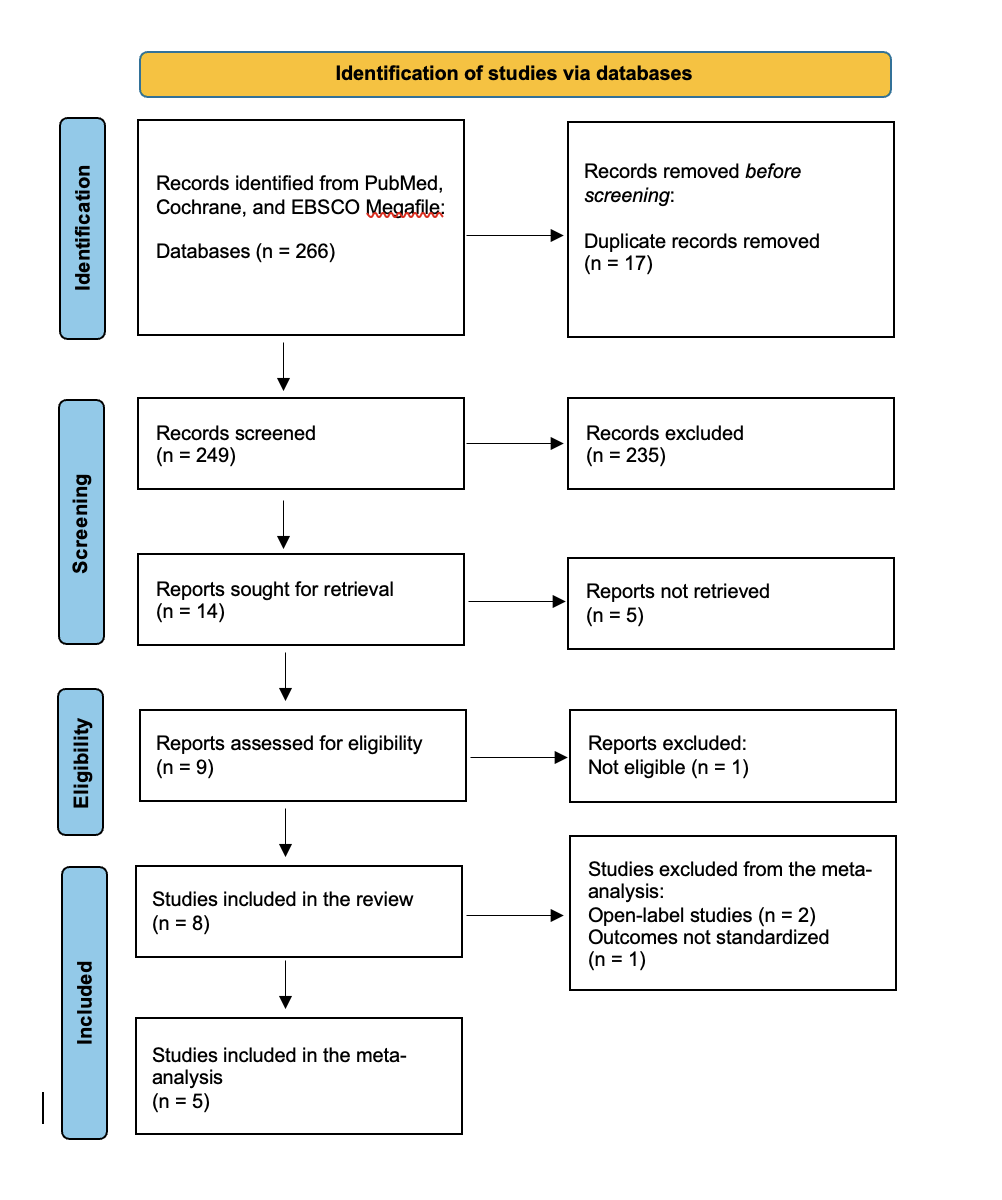
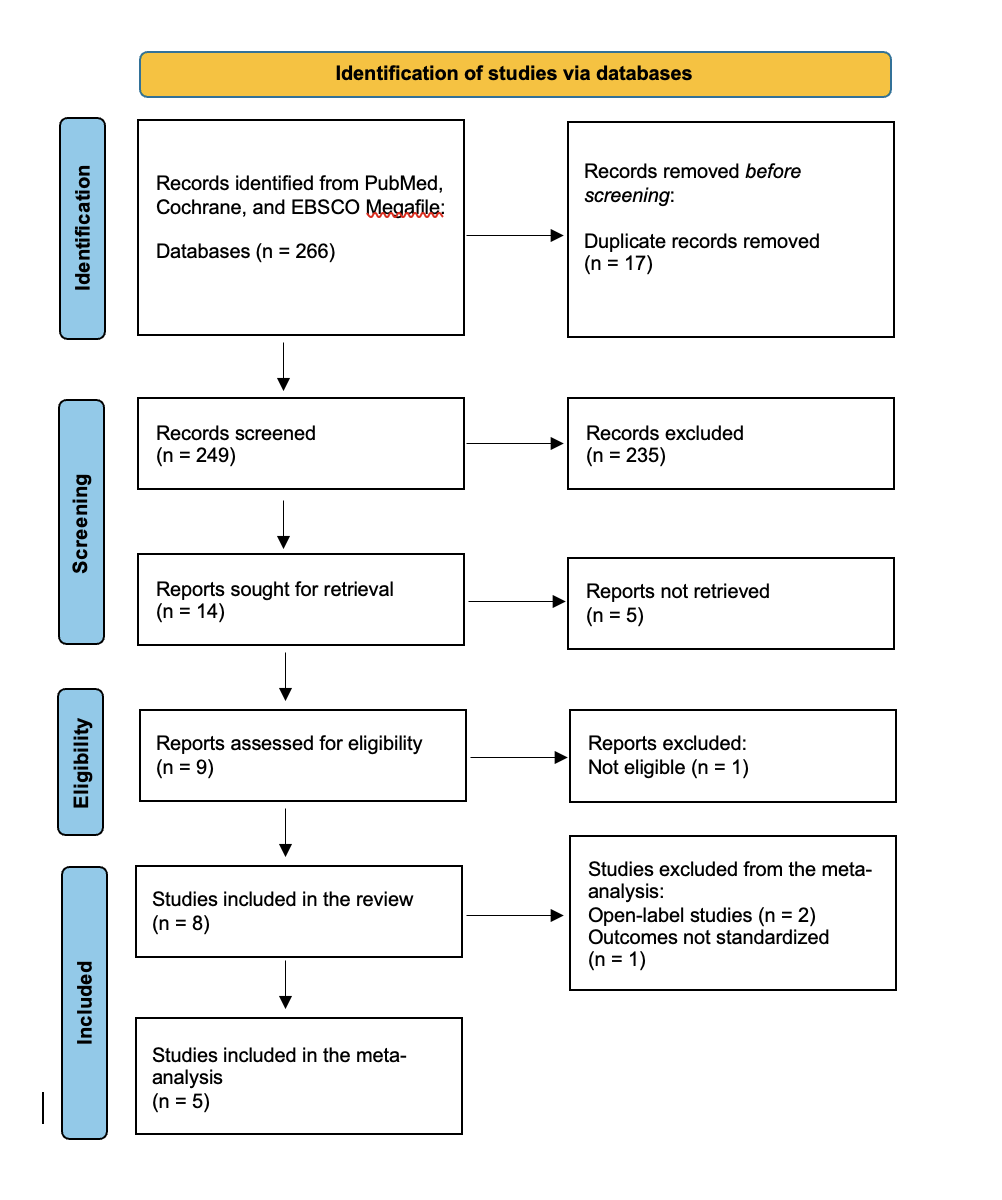
Background: Parkinson’s Disease (PD) is a progressive neurodegenerative disorder characterized by motor fluctuations and dyskinesias that become increasingly challenging to manage in advanced stages. Continuous subcutaneous Apomorphine infusion offers a less invasive alternative to device-aided therapies such as deep brain stimulation and Levodopa-Carbidopa intestinal gel. This systematic review and meta-analysis aimed to evaluate the efficacy of Apomorphine infusion in reducing OFF time and motor symptom severity, focusing on Unified Parkinson’s Disease Rating Scale (UPDRS) Part III scores in individuals with advanced PD. Objectives: A systematic search of PubMed, Cochrane, and EBSCO Megafile databases was conducted through April 16, 2025, according to PRISMA guidelines. Randomized controlled trials (RCTs) evaluating Apomorphine infusion and reporting outcomes on OFF time and UPDRS Part III were included. Risk of bias was assessed using the Cochrane RoB 2 tool, and certainty of evidence was evaluated with GRADE. Meta-analyses were performed using a random effects model. Result: Eight studies (n = 458) met the inclusion criteria, of which five were eligible for meta-analysis. Apomorphine infusion significantly reduced OFF time compared to placebo (MD = -1.93 hours; 95\% CI: -2.91 to -0.95; low-certainty evidence), with minimal heterogeneity (I² = 0\%). A significant reduction was also observed in UPDRS Part III scores (MD = -19.11; 95\% CI: -25.54 to -12.68; very low-certainty evidence), although substantial heterogeneity was present (I² = 67.93\%). Conclusion: This systematic review supports the efficacy of Apomorphine infusion in reducing OFF time and improving motor symptoms in individuals with advanced PD. Apomorphine infusion represents a treatment option, particularly for patient’s ineligible for surgical interventions. However, the overall certainty of evidence is limited by methodological heterogeneity and a small number of high-quality trials. Future studies should aim for standardized outcome measures, long-term comparisons with other device-aided therapies, and exploration

Introduction: The COVID-19 pandemic has dramatically accelerated the adoption of telemedicine across various medical disciplines, including psychiatry. In Norway, however, this trend did not naturally extend to psychiatric services, particularly in the area of ADHD assessments, which continued to experience heightened demand and extended waiting lists. This situation is exacerbated by a shortage of healthcare providers specialized in ADHD, leading to lower prioritization of ADHD assessments in public healthcare services. Additionally, Norway's geographical size and diverse climate conditions presents another layer of complexity. Access to specialized diagnostic centers is particularly challenging for patients residing in remote locations. This circumstance contributes to the increased complexity of ADHD assessmentObjective: The primary objective of this experience was to investigate the efficacy and efficiency of a telemedicine-based approach for diagnosing Adult Attention Deficit Hyperactivity Disorder (ADHD) in Norway. Given the existing barriers—long waiting lists, scarcity of specialized healthcare providers, and geographical constraints—the experience aimed to streamline the diagnostic process. By leveraging digital technology, we intended to expedite assessments, improve accessibility for patients in remote areas, and maintain the diagnostic rigor typically associated with in-person evaluations.Methods: In this experience, we employed a digital team-based approach to conduct ADHD assessments in a single, intensive session. Our team consisted of a psychiatrist and a psychiatric nurse specialized in ADHD. This session was designed to be time compressed, conducted over approximately 3 hours in a single day, through a digital platform. This intensive approach was designed to streamline the assessment process, making it more accessible and time-efficient for patients. Pre-Assessment Screening: Several days before the digital encounter, candidates underwent a pre-assessment screening process. The inclusion criteria were adults aged 18 or above, with no severe psychiatric history or substance abuse. Candidates were required to complete and submit a series of questionnaires and blood tests.Digital Encounter: The evaluation was carried out entirely via a secure online platform, utilizing a computer as the primary interface. A significant portion of this digital session involved a psychiatric interview and associated evaluations, lasting approximately 3 hours in total. During this time, a digital MOXO d-CPT test was also administered to the patient. Due to the inability to maintain uninterrupted visual contact using the computer's camera during the MOXO test, patients were instructed to place a mobile device at an approximate distance of three meters from themselves. This mobile device was then used for maintaining contact via WhatsApp or FaceTime with us, allowing the clinical team to continue with uninterrupted, ongoing visual observation of the patient during the MOXO test as well.Results: During our study, the specialized ADHD assessment team successfully conducted evaluations for a cohort comprising 52 patients. In this group, 43 patients (82.7%) were diagnosed with ADHD upon a single digital consultation, while an additional 4 patients (7.7%) received their diagnosis over the course of multiple appointments. ADHD was confidently ruled out in 3 patients (5.8%) after just one appointment, and in 2 patients (3.8%) after multiple appointments. In summary, 47 patients (90.4%) were diagnosed with ADHD, whereas 5 patients (9.6%) were excluded from this diagnostic category.Digital evaluations took more time than traditional in-person assessments, with an average increase of 15 minutes. Conclusions: The specialized and digital approach adopted for ADHD assessments has proven to be an effective and promising alternative. While digital assessments did require a slightly increased time investment compared to in-person evaluations, the substantial advantages of this approach—such as its ability to reach patients in remote locations, the reduction of carbon footprint associated with travel, and patient comfort—make this extra investment of time entirely warranted. In summary, our specialized and digital approach not only validates its diagnostic effectiveness but also emphasizes how innovation can effectively address critical challenges in modern ADHD assessment. This method emerges as a valuable tool for streamlining and enhancing the diagnostic process for individuals seeking ADHD assessment.
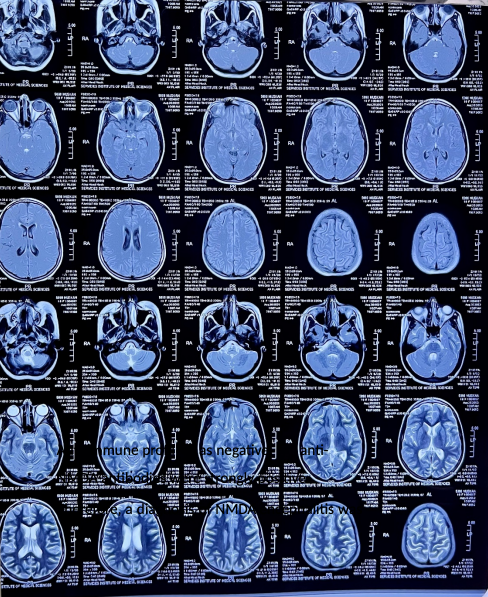
Background: Anti-NMDA receptor encephalitis is a rare autoimmune disorder caused by the formation of antibodies against NMDA receptors in the brain. Symptoms can include confusion, hallucinations, seizures, memory loss, and difficulty speaking, as well as autonomic dysfunction and movement disorders.Case Presentation: The case presented is of an 18-year-old female patient who presented with altered behavior, low-grade fever, and rigidity. The patient was diagnosed with NMDA encephalitis based on elevated protein levels, lymphocytes pleocytosis, and positive NMDA antibodies in serum. The patient was treated with pulse therapy with injection Solumedrol and IVIGs, leading to significant improvement. No underlying cause for the encephalitis was identified.Conclusion: The diagnosis is typically made through a combination of clinical findings, laboratory tests, and imaging studies, and the detection of anti-NMDA receptor antibodies in the cerebrospinal fluid (CSF) and serum. Treatment typically involves immunotherapy, such as steroids or plasma exchange, and treatment of any underlying infection or tumor. Prognosis varies based on the severity of the disorder and timing of treatment, with early diagnosis and treatment leading to better outcomes. This case highlights the importance of early diagnosis and treatment of anti-NMDA receptor encephalitis for a better outcome.
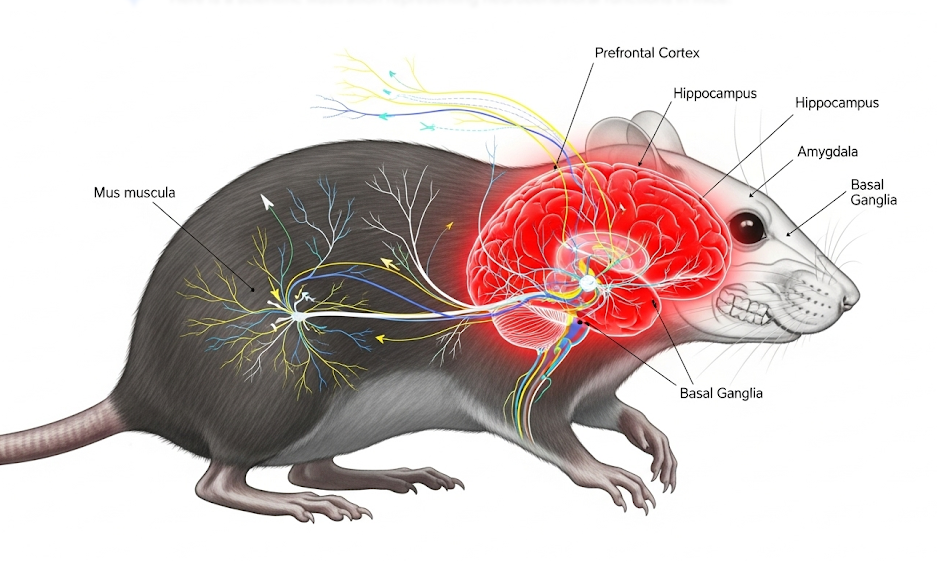
Background: Organophosphate compounds represent a major class of chemicals commonly applied in agricultural pest control [5]. Most studies of moderate pesticide exposure have found an increased prevalence of neurological symptoms and changes in neurobehavioral performance, which reflects cognitive and psychomotor dysfunction [2]. Glyphosate (GLY) is the active ingredient of the most used herbicide worldwide [1]. Pituitary adenylate cyclase-activating polypeptide (PACAP) is a 38- amino-acid neuropeptide that belongs to the secretin/glucagon/vasoactive intestinal peptide (VIP) [3]; [4]. Several in vitro and in vivo studies revealed that PACAP exerts its neuroprotective properties. Anxiety and depression are highly co-morbid with each other. This research aims to study the toxicity of GLY and the effect of the neuropeptide PACAP, accompanied by behavioral studies to test anxiety and depression.Materials/Methods: In vivo, a sexually mature male Swiss albino mice model with repeated exposure to GLY and/or PACAP for 15 days elicited evident emotional behavioral alterations as assessed by several behavioral tests after 48 hours of stopping treatment. Four tests were performed. The elevated-plus-maze test is used to assess anxiety-like behavior in rodents as well as the open field test to further assess locomotor activity and emotional reactivity. The tail suspension and the dark/light box tests are used to evaluate potential antidepressant-like effects. The apparatus was cleaned with a solution of ethanol of 10 % between tests to remove animal odors. Time was recorded using a video camera and analyzed by the Ethovision XT Noldus 8.5 video tracking program. All results were analyzed using GraphPad Prism 8.0 (GraphPad Software Inc.). The data are represented as the mean ± standard deviation (SD) of at least three independent experiments when shown as a bar graph. Statistical comparisons were performed between the control and treatment groups using Tukey's post hoc test for multiple comparisons of one-way analysis of variance. p < 0.05 indicated significantly difference (*); P<0.01 difference is extremely significant (**) and p<0.001 difference is highly significant (***).Results: Repeated exposure to GLY and/or PACAP for 15 days elicited evident emotional behavioral alterations in mice, as assessed first by the Tail Suspension Test (TST) in which the total time spent immobile during the last 4 minutes of a session was scored to evaluate potential antidepressant-like effects in mice. The statistical analysis of the immobility time recorded of the TST showed that the glyphosate group presented an increase in the percentage of immobility time compared to the control indicating an elevation of depressive-like behavior in that group (highly significant **). However, compared to the glyphosate group, the co-treated group demonstrated a decrease in immobility time (compared to the Glyphosate group) illustrating the effects of PACAP in alleviating depressive-like behavior. Second, for the dark/light box test in two-chambered systems, where animals can freely move between brightly lit open fields and dark corners, mice show more crossings between two chambers and more locomotor activity after treatment with GLY. The time spent in the bright compartment was an extremely significant (****) increase for the two treatments with the herbicide and with the neuropeptide compared to control groups and an extremely significant (####) decrease in the PACAP group compared to the Glyphosate group. We recovered 11 boli of mice feces and urine from the herbicide-treated group, eight boli for the PACAP group seven boli from the co-treated groups, and nothing from the control group. Then, for the elevated-plus-maze test, the time spent in open arms is used as indices of open space-induced anxiety. The percent of entries and time spent in each arm constitute the index of primary anxiety. The analysis of the ratio of open arm (OA) entries showed a slight decrease in several entries compared to the control group, which is statistically insignificant. Similarly, the glyphosate group spent less time exploring the OA. On the other hand, the GLY + PACAP group spent a moderate amount of time exploring the OA. We can deduce that anxious mice spend little time in the open arms and make very few entries into the open arms. The anxiety index showed that treatment with PACAP relieves depression behavior. Ultimately, we performed the Open field test which consists of placing an animal in an unknown environment with surrounding walls, to observe behavior patterns including: ? The tendency to stay on the periphery of the field without entering the center (called thigmotaxis) and often interpreted as anxious behavior. ? Level of defecation and urination, in which I recovered 10 boli of feces for the group treated with GLY and 7 boli for the co-treated groups, and nothing recovered for the control and PACAP-treated groups. Therefore, the time spent in the center area is an index of anxiety behavior, this test assesses locomotor activity and emotional reactivity. Conclusion: With the widespread use of pesticides, the impact of pesticides on host health has received more and more attention. Glyphosate exposure induced an exacerbation of anxiety and depression-like behaviors and treatment with PACAP alleviate it. Our findings provide strong evidence that the neuropeptide PACAP can be used as a novel treatment option for neurological disorders and provide novel insights into the mechanism underlying glyphosate-induced health risks, particularly mood disorders.
Introduction: Pneumocephalus is a rare phenomenon, typically resulting from traumatic or non-traumatic causes. It could however occur spontaneously, in the absence of an underlying condition or from manipulation of a venous catheter resulting in retrograde movement of air against the direction of blood flow causing fatality [1-4]. It occurs in less than 3 per 100,000 hospitalizations [5]. This case reports possible etiologies of a rare case of pneumocephalus resulting in a stroke. Materials and Methods: A review of chart and verbal consent from patient’s family prior to reporting case.Results and Discussion: We present a 76-year-old African American female with End Stage Renal Disease who presented to the ED for altered mental status, following an episode of bleeding during a hemodialysis (HD) completed via the internal jugular vein through a tunneled dialysis catheter. Neurological examination revealed signs of a massive stroke including a right lateral gaze, with 3+ reflexes in the upper extremities bilaterally. Head CT scan revealed moderate amounts of air within the right frontoparietal sulci, minute intraparenchymal foci of gas within the venous structures; interval gray-white loss involving the right frontoparietal lobe and right centrum semiovale, with watershed involvement. Echo cardiogram revealed no wall or valvular defect. She was not deemed appropriate for Hyperbaric oxygen and discharged to a palliative care facility by family. Conclusions: While some causes of pneumocephalus have previously been documented in literature, unusual etiology can lead to diagnostic dilemma and calls for a high level of suspicion by healthcare providers
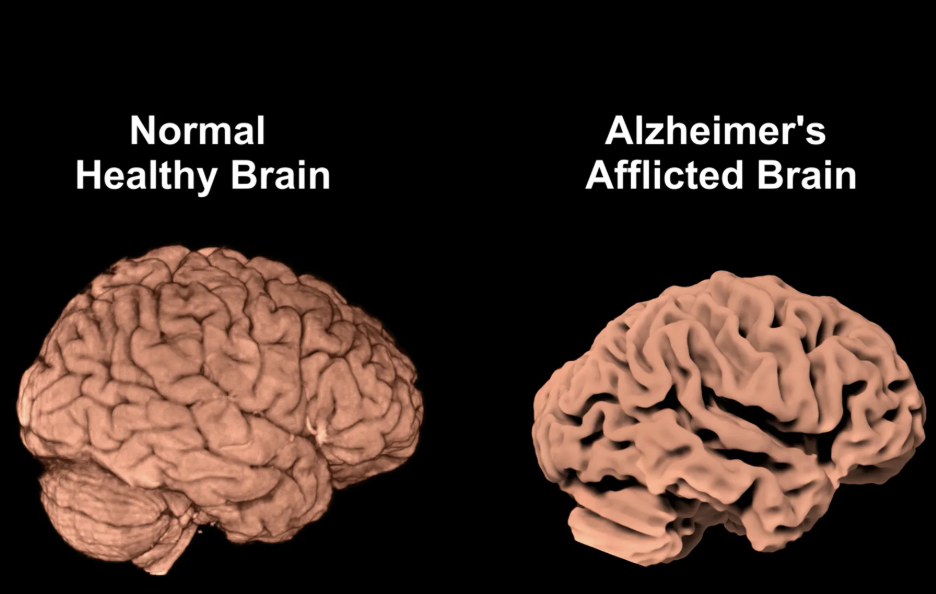
The integration of artificial intelligence (AI) and digital health solutions into neurology represents one of the most promising transformations in modern medicine [1]. As neurological disorders continue to account for a substantial burden of disease worldwide, the convergence of advanced computational tools, digital monitoring systems, and patient-centered health technologies offers the opportunity to redefine how neurological care is delivered, monitored, and optimized [2].AI in Diagnosis and Prognosis One of the most impactful applications of AI in neurology lies in diagnostic imaging and predictive analytics [3]. Machine learning algorithms are now capable of analyzing brain magnetic resonance imaging (MRI) and computed tomography (CT) scans to detect subtle pathological features that may be overlooked by the human eye. For example, convolutional neural networks have been trained to identify early-stage Alzheimer’s disease by detecting hippocampal atrophy patterns, enabling diagnosis years before clinical symptoms manifest [4]. Similarly, AI systems are being applied to detect ischemic stroke with remarkable speed and accuracy, facilitating rapid triage in emergency settings [5]. These tools not only reduce diagnostic delays but also enhance prognostic predictions by integrating multimodal datasets such as neuroimaging, genetics, and clinical history [6].Digital Biomarkers and Remote Monitoring Beyond diagnosis, digital health tools are transforming how neurologists monitor disease progression. Wearable devices, smartphones, and sensor-based platforms provide continuous, real-world data on motor activity, speech, gait, and sleep quality [7]. In Parkinson’s disease, accelerometer-based wristbands can quantify tremors and bradykinesia, while voice analysis apps detect subtle speech impairments associated with disease progression. Similarly, in multiple sclerosis, smartphone-based assessments of hand dexterity and balance allow clinicians to remotely track functional decline. These digital biomarkers provide granular, objective data that complement clinic-based assessments, enabling earlier therapeutic adjustments and more personalized care [8].Telemedicine and Access to Care The COVID-19 pandemic accelerated the adoption of telemedicine, highlighting its role in neurology where access to specialists is often limited. Digital platforms have allowed neurologists to assess stroke recovery, perform cognitive testing, and deliver psychiatric support virtually. For patients in remote or underserved regions, tele-neurology bridges geographic barriers and reduces waiting times for specialist consultations. Moreover, integration of AI into telemedicine platforms—for example, automated triaging systems or AI-assisted neurological examinations—enhances efficiency and clinical decision-making [3].AI in Clinical Research and Therapeutics The role of AI is also expanding into clinical trial design and therapeutic discovery. By mining large-scale datasets, AI can identify potential drug targets, predict treatment responses, and stratify patients for clinical trials. In epilepsy research, AI algorithms analyzing electroencephalography (EEG) data have shown promise in predicting seizure onset, paving the way for precision medicine interventions [5]. Likewise, digital therapeutics such as smartphone-based cognitive training programs or virtual reality for neurorehabilitation are emerging as adjunctive treatment modalities validated through clinical research [6].Ethical and Practical Considerations Despite these advances, significant challenges must be addressed for widespread adoption. Data privacy remains a paramount concern, particularly when sensitive neurological data such as brain scans or genetic information are collected and stored digitally [2]. Regulations such as the General Data Protection Regulation (GDPR) in Europe emphasize the importance of safeguarding patient confidentiality, but global standards remain fragmented. Additionally, algorithmic transparency or the “black box” problem of AI—poses ethical dilemmas when clinical decisions are based on models whose reasoning cannot be easily explained [7].Another critical concern is health equity. Many digital health tools are developed and validated in high-income countries, raising questions about their applicability in resource-limited settings. Without deliberate efforts to ensure inclusivity, there is a risk of widening the digital divide, leaving vulnerable populations without access to these innovations [8]. Therefore, collaboration among clinicians, engineers, policymakers, and patient advocacy groups is essential to ensure equitable deployment of AI and digital health tools [4].The Future of Neurology with AI and Digital Health Looking forward, the synergy of AI and digital health promises to enable precision neurology where diagnosis, treatment, and monitoring are tailored to the individual patient in real time [1]. Integration of multimodal data streams including genetics, lifestyle factors, imaging, and wearable-derived biomarkers will facilitate holistic, personalized care [6]. Furthermore, advances in natural language processing may soon enable AI systems to analyze patient speech during clinical encounters, automatically generating clinical documentation and identifying cognitive or psychiatric symptoms [3].In neurorehabilitation, AI-guided robotics and virtual reality programs are already demonstrating improved motor recovery in stroke patients [5]. Similarly, predictive analytics may allow proactive interventions for patients at risk of relapse in conditions such as multiple sclerosis or schizophrenia [7]. The combination of continuous patient-generated data with clinician oversight will move neurology from a reactive to a proactive discipline, focusing on prevention and early intervention rather than late-stage management [8].Conclusion In conclusion, the integration of AI and digital health into neurology represents a paradigm shift with profound implications for clinical practice, research, and patient care [2]. While challenges related to privacy, ethics, and access remain, the potential benefits including earlier diagnosis, continuous monitoring, personalized treatment, and broader access to care are undeniable. The future of neurology will not be shaped by technology alone but by how effectively neurologists, patients, and society embrace and guide these innovations [4]. Responsible adoption will require interdisciplinary collaboration, robust regulatory frameworks, and a steadfast commitment to patient-centered care [1].

Latvia currently does not have a dedicated educational website for patients living with Parkinson’s Disease (PD). This absence leaves patients and caregivers without a trusted source of information in Latvian. Many patients I have spoken with describe struggling to find guidance on daily management, medication use, and non-motor symptoms such as fatigue, anxiety, or sleep disturbances. Beyond clinical visits, there is little support available, and this gap adds to feelings of isolation and uncertainty. To address this, I am taking the initiative to create the first national educational website for patients with PD in Latvia. This platform will provide reliable, evidence-based materials in Latvian, designed specifically for patients and caregivers. It will cover practical strategies for living with PD, information on both motor and non-motor symptoms, and resources that patients can trust as they navigate their diagnosis. In other countries, online resources of this kind are an essential first step in patient support [1,2]. Research shows that educational platforms help patients feel more informed, more confident in managing their condition, and less alone [3,4]. They also provide healthcare professionals and policymakers with a window into patient needs, making care more responsive and patient-centered [5]. This website will: • Be the first central, trusted resource for PD patients in Latvia. • Offer clear, evidence-based content in Latvian. • Be freely accessible to patients and caregivers across the country, including those in rural areas. • Serve as a foundation for future initiatives, such as online events or interactive support features. The creation of a national educational website will mark the first coordinated effort to provide Latvian patients with PD and their families with accessible, trustworthy information. I am committed to ensuring that this resource is developed and made available where it is most needed. Sincerely, Paula Abola
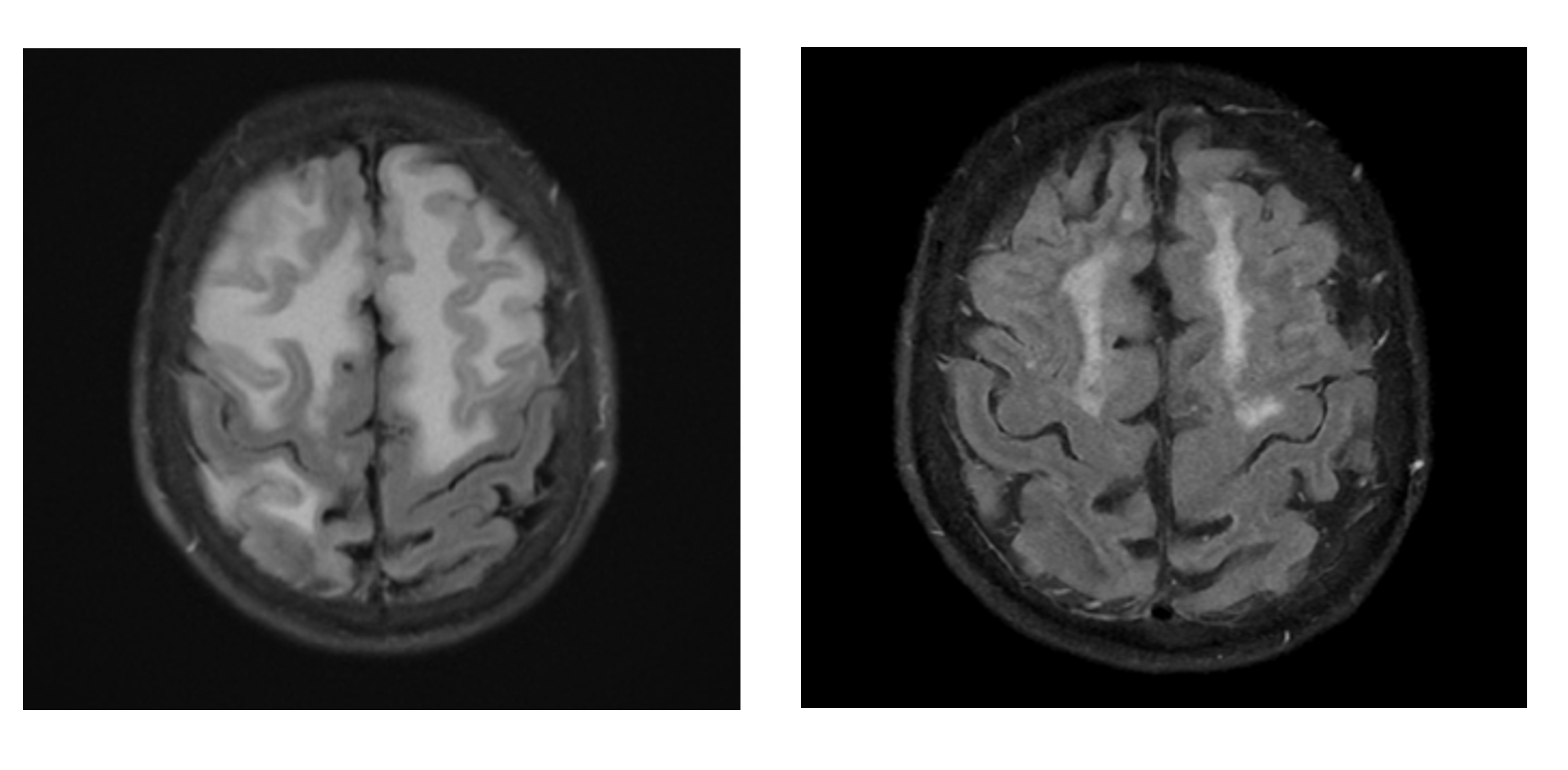
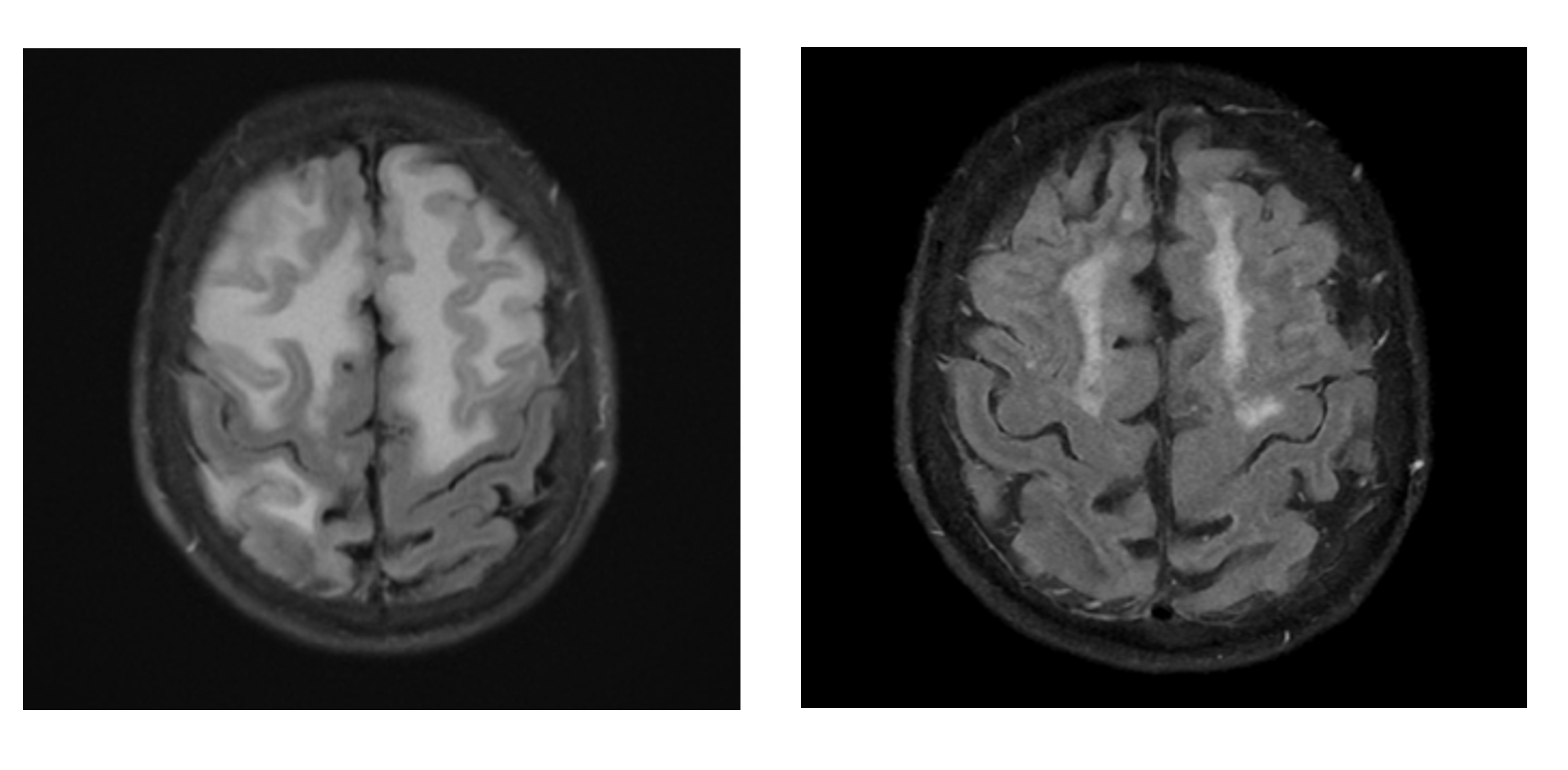
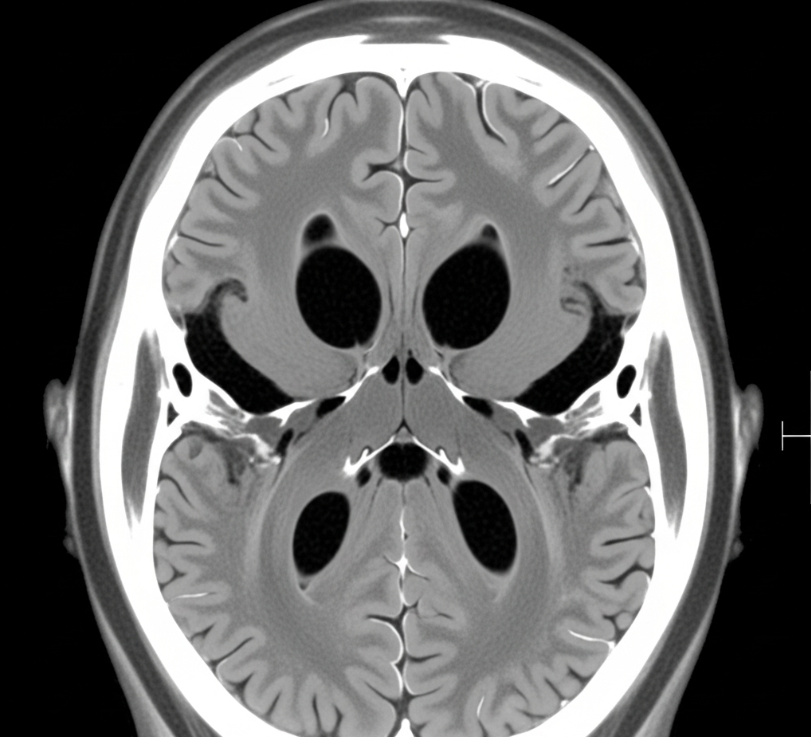
Objective: To highlight the diagnostic and therapeutic importance of recognizing inflammatory cerebral amyloid angiopathy (iCAA) presenting with atypical cognitive decline and evolving neuroimaging findings.Background: Cerebral amyloid angiopathy (CAA) is an age-associated disease characterized by gradual deposition of beta-amyloid within the walls of cortical and leptomeningeal vessels. The inflammatory variant (iCAA) can cause subacute encephalopathy, seizures, and headaches with asymmetric white matter edema that can be steroid responsive. Diagnostic delays can occur due to the slow evolution of disease and overlap with more prevalent pathologies.Results: An 84-year-old woman initially presented with progressive aphasia. Brain MRI revealed lobar hemorrhage, T2 FLAIR white matter changes, and widespread cortical microbleeds. She was diagnosed with primary intracerebral hemorrhage but was lost to follow-up. Several years later, she returned with acute encephalopathy, worsening cognitive function, and radiographic changes that were inconsistent with previous explanations. The extensive workup for infectious and neoplastic conditions was unremarkable. Repeat imaging revealed persistent cortical microbleeds alongside new vasogenic edema—now fulfilling Boston Criteria 2.0 for probable CAA, with rising concern for an inflammatory variant. A brain biopsy was considered but deferred. High-dose IV methylprednisolone was initiated empirically, followed by an oral prednisone taper. Within weeks, she showed rapid clinical recovery, and follow-up MRI confirmed resolution of vasogenic edema with no new hemorrhages. Two months later, she regained baseline cognitive function and was independently performing daily tasks.Conclusions: This case illustrates how evolving radiologic patterns, when paired with unexplained clinical decline, can unmask a treatable diagnosis. iCAA mimics alternate pathologies but responds dramatically to immunosuppression. Delay in recognition can cost precious recovery time. Early identification, grounded in evolving imaging and clinical suspicion, can lead to cognitive improvement. Clinicians must remain vigilant to evolving MRI patterns and unexplained cognitive changes, particularly when prior diagnoses fail to account for clinical reality.
We commend the study, “Efficiency of Topical Rifampin on Infection in Open Neural Tube Defects: A Randomized Controlled Trial,” recently published in The International Journal of Neuroscience, for its valuable insights into infection prevention in open neural tube defects (NTDs). However, several aspects warrant further discussion to enhance the robustness and applicability of the findings. The study does not specify the follow-up duration, a critical omission as ventriculoperitoneal (VP) shunt-related infections may develop over time. Extending the follow-up could provide a more comprehensive evaluation of rifampin’s long-term efficacy and safety. Furthermore, although no adverse effects were reported, the study lacks details on monitoring procedures, limiting conclusions about rifampin’s safety profile. Another concern is the significantly higher rate of cerebrospinal fluid (CSF) sac ruptures in the rifampin group (p=0.006). The absence of discussion regarding potential causes and clinical relevance of this finding requires further investigation. Additionally, the study’s focus on paraplegic newborns with open NTDs raises questions about generalizability. A broader inclusion, as seen in another study addressing paraplegic and non-paraplegic cases, found meningitis or VP shunt infections in 6.7% and surgical site infections (SSI) in 3.3% of patients treated with topical rifampin. Clarifying these issues, particularly regarding long-term outcomes, adverse event monitoring, and generalizability, would strengthen the study’s conclusions. Addressing the implications of CSF sac rupture rates is also crucial. We hope these observations contribute to ongoing research in this important area.
Central nervous system infections (CNSI) are severe, life-threatening conditions that require rapid and accurate diagnosis for effective management. To address diagnostic challenges in CNSI, molecular diagnostic tools have been developed to improve the detection and identification of CNS pathogens.Objectives: This study aims to assess the diagnostic accuracy of the BioFire® FilmArray® Meningitis/Encephalitis (ME) Panel in detecting CNS pathogens and compare its performance with cerebrospinal fluid (CSF) culture and single-target polymerase chain reaction (PCR).Methods: A systematic literature search identified studies published between 2016 and 2024. Data were analyzed and evaluated the Cochrane RevMan Web.Results: Twenty-three studies were included with a total of 11,182 patients. The ME Panel exhibited high accuracy for viral pathogens, with an average sensitivity of 97% and specificity of 99.8%, particularly for Enterovirus, Herpes Simplex Virus (HSV), and Varicella Zoster Virus (VZV). Bacterial detection showed greater variability, with a pooled sensitivity of 89% and specificity of 99.6%, highlighting challenges in detecting S. pneumoniae and L. monocytogenes. Sensitivity for Cryptococcus was lower at 70%, although specificity remained high at 99%.Conclusion: The ME Panel provides rapid and accurate detection of CNSI, facilitating timely treatment decisions. However, its cost and limited pathogen coverage may hinder its use in resource-limited settings.
Mycobacterium tuberculosis accounts for 5.9% of central nervous system infection which may take 1 of 3 clinicopatholgical forms including tubercular meningitis, Central Nervous System tuberculoma and spinal arachnoiditis. This case series reports three cases of extrapulmonary nervous system tuberculosis accounting for approximately 1–2% of all Tuberculosis cases and 10% of musculoskeletal TB cases. Incidence rates in immunocompetent versus immunocompromised individuals significantly varies but increasing number of immunocompetent individuals being affected by the diseases has increased over the past decade presenting in unusual locations.We report cases involving three immunocompetent patients diagnosed with extra- pulmonary tuberculosis found in the rare locations and presented with varying clinicalpresentations. All patients underwent standard medical therapy and individualized surgical interventions based on disease location and severity.
Binge eating disorder (BED) is the most common eating disorder and is associated with obesity, metabolic comorbidities, and psychiatric burden. While psychotherapy remains the first-line treatment, pharmacologic options are increasingly explored. Topiramate, an antiepileptic drug with appetite-suppressing and satiety-enhancing properties, has been investigated in randomized controlled trials (RCTs) for BED.ObjectivesThis meta-analysis aimed to determine the efficacy of topiramate in BED. Specifically, we evaluated its effects on binge frequency and weight outcomes.MethodsWe systematically searched PubMed, Cochrane, and ClinicalTrials.gov through September 2025 for RCTs evaluating topiramate in BED. Eligible trials compared topiramate with placebo in adults with BED or bulimia nervosa. Data on binge frequency, abstinence rates, and weight change were extracted. Risk of bias was assessed with Cochrane criteria. Random-effects models were used to pool outcomes.ResultsFour RCTs with 550 participants were included. Topiramate significantly reduced binge eating frequency compared to placebo, with a pooled mean difference of 1.35 (95% CI: 0.71–1.99; p =
Delirium is defined as a neurological incapacity that is acute in nature and usually subside after some time. It is one of the most serious metabolic disorders that is usuallyattributedtoawiderangeofcomplications.Deliriumhasbeenlinkedtodualorexin receptor antagonists (DORAs); medications commonly prescribed to treat insomnia. The objective of this study is to evaluate the efficacy of DORAdrugs, Suvorexant and Lemborexant in delirium prevention. Methods: We conducted a literature search on PUBMED, EMBASE, and Cochrane Library electronic databases among others from inception to September 1, 2024. Published papers on dual orexin receptor antagonists (DORA) in delirium prevention that have met the eligibility criteria were included for data extraction and quality assessment. Results: From the evaluated studies with 930 patients of who 132 were on Suvorexant and 58 on Lemborexant. We pooled this evidence and identified that the incidence of delirium is significantlylow in patients treated with Dora medications as compared to non-users. Conclusions: Dual orexin receptor antagonists were effective in preventing delirium in critically ill patients. Prospective studies are needed for confirmation of these results and evaluation of the effect of the drugs on the death rates in the hospital, their effect on the duration of stays in the ICU and the days that the patients are under mechanical ventilation.
Alcohol use disorder (AUD) is a medical condition characterized by an impaired ability to stop or control alcohol use despite known consequences. There is difficulty in achieving both in initiation and maintenance of abstinence, which have been a constant challenge for the treating physician as well as the patient. An adjunct treatment to reduce dependence on pharmacotherapy or increase adherence to currently used medications for AUD is definitely needed. Repetitive Transcranial Magnetic Stimulation (rTMS) is a noninvasive procedure that uses the principles of magnetic fields to stimulate a specific area of the brain to improve symptoms. Methods. PubMed, Cochrane, Embase, and ClinicalTrials.gov were searched for articles from inception to 15 August 2024. Data were analyzed using Cochrane RevMan Web. Odds ratio (OR), mean difference (MD), and 95% confidence intervals (CI) were combined via fixed-effect analysis. Results. Three randomized controlled trials were included with a total of 140 patients. Repetitive Trans-cranial Magnetic Resonance stimulation could reduce alcohol dependence of Alcohol Use Disorder patients at endpoints (OR 0.12, 95% CI [-0.40, 0.64] but the results are not significantly different from the control group. However, all three RCTS have shown significant decrease in alcohol cravings in patients receiving treatment of rTMS on the left prefrontal cortices. Conclusions. Repetitive Trans-cranial Magnetic Resonance stimulation shows no significant difference from control in the reduction of alcohol dependence among patients with Alcohol Use Disorder. However, there was noted decrease in alcohol cravings after rTMS intervention among patients with AUD when applied on the left prefrontal cortex.

Parkinsonism is a syndrome characterized by bradykinesia, rigidity, tremor, and postural instability, with Parkinson’s disease (PD) being the most common cause. Increasing evidence suggests that infectious diseases may play a role in triggering or exacerbating Parkinsonian symptoms through direct neurotoxicity, neuroinflammation, or alterations in the gut--brain axis. \textbf{Methods:} A scoping review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines was conducted. PubMed, Cochrane, and MEDLINE databases were searched for studies examining infections, PD, and Parkinsonism. Eligible studies assessed infection-related PD or Parkinsonism risk and symptom modulation. \textbf{Results:} Thirty-seven studies met the inclusion criteria. Several infections were linked to Parkinsonism, with chronic viral infections such as hepatitis C virus (HCV) and hepatitis B virus (HBV), and bacterial infections including \textit{Helicobacter pylori} and \textit{Clostridium difficile}, associated with an increased risk of PD, while some infections showed no significant effect. Acute infections, such as urinary tract and respiratory infections, were frequently linked to transient worsening of symptoms. Antiviral therapy and \textit{H. pylori} eradication demonstrated potential benefits, although findings were inconsistent. \textbf{Conclusion:} The relationship between infections and PD is complex, with certain infections potentially triggering or worsening symptoms, while others appear neutral or protective. Understanding infection-related mechanisms of neurodegeneration is essential for developing preventive and therapeutic strategies. Further longitudinal studies are needed to clarify causal links and optimize infection management in PD.
